Kananelo Boloetse
Cervical cancer ranks number one most frequent cancer among women with 541 diagnosed yearly resulting in 362 annual deaths due to late diagnosis and treatment, the latest World Health Organisation (WHO) report reveals.
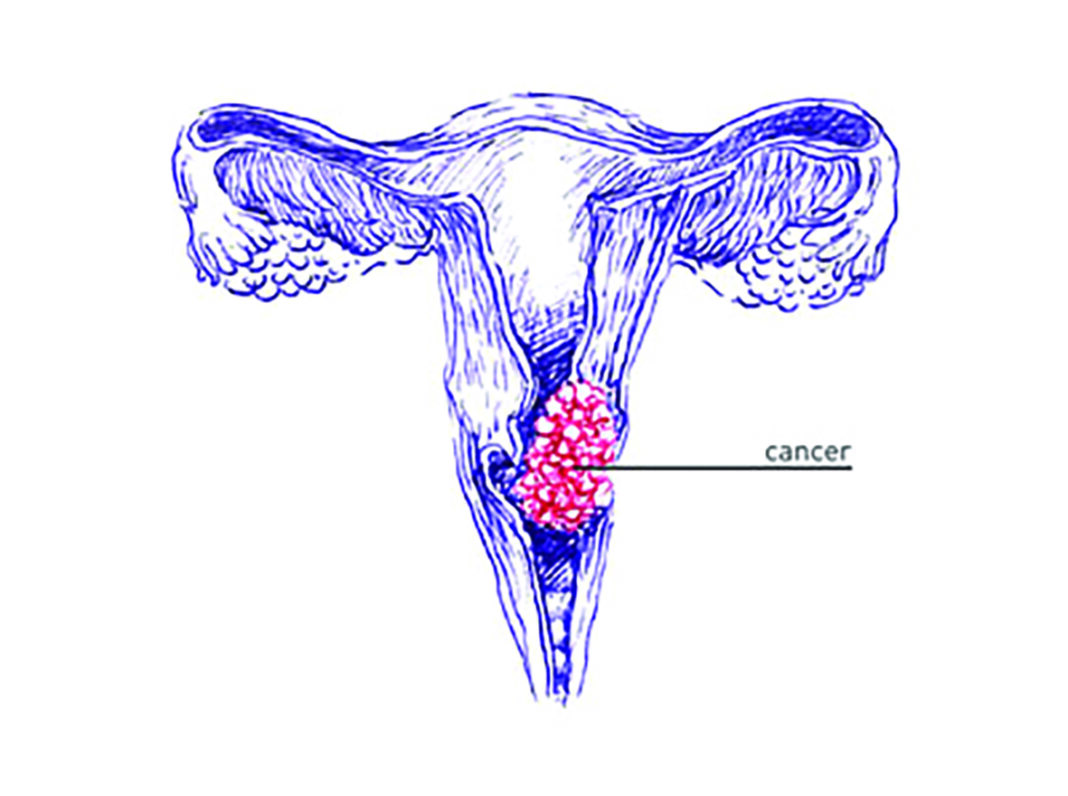
Cervical cancer, according to WHO, develops in a woman’s cervix, the entrance to the uterus from the vagina
It says almost all cervical cancer cases (99 percent) are linked to infection with high-risk human papillomaviruses (HPV), an extremely common virus transmitted through sexual contact.
Although most infections with HPV resolve spontaneously and cause no symptoms, persistent infection can cause cervical cancer in women.
It is the most common kind of cancer in Lesotho with one of the highest incidence rates in the world.
The annual report, published by WHO on Wednesday this week, estimates that Lesotho has a population of about 700,000 women above 15 years who are at risk of developing cervical cancer.
It suggests that while there may be several opportunities available to prevent the development of cervical cancers (safe sexual practices and delay in onset of sexual activity), the single most effective early prevention strategy is HPV vaccination.
“… HPV vaccination prevents over 95 percent of the HPV infections caused by HPV serotypes 16 and 18 as well as a cross-protection against other less common HPV serotypes which cause cervical cancer,†reads the report.
Lesotho successfully reintroduced the HPV vaccine in 2022 for all adolescent girls aged 9-14 years old, according to the report.
Over 370 health workers across the country were trained with support from the WHO country office before the launch of the vaccination campaign.
“The reintroduction of the vaccine brought together many stakeholders (Ministry of Education and Training, Heads of schools and communities) together for macro-planning/microplanning, development of campaign messages, readiness assessment and trainings of vaccinators and supervisors,†it reads.
It adds: “A total of 91,140 (71.9 percent) out of 126,761 were vaccinated in all the ten districts over three weeks. Given the context of the prevailing COVID-19 pandemic, the coverage was considered a success.â€
WHO country representative, Dr Richard Banda, said the annual report gives an overview of the WHO Lesotho country office’s undertakings and achievements in the context of an extraordinary health emergency.
“As we walk another mile this year, may we embrace all lessons learned in the previous year, learn from what did not work so well, and take on new opportunities in championing health in the country,†Dr Banda said.
He thanked the Government of Lesotho and all stakeholders who continue to work tirelessly to create a healthier society daily.
“We have a bold commitment to accelerate progress and build forward a society that places health at the centre of development,†he said.
Worldwide, cervical cancer is the fourth most frequent cancer in women with an estimated 604,000 new cases in 2020, WHO said in February last year.
It mentioned that of the estimated 342,000 deaths from cervical cancer in 2020, about 90 percent of those occurred in low- and middle-income countries.
It further stated that women living with HIV were six times more likely to develop cervical cancer compared to women without HIV, and an estimated five percent of all cervical cancer cases were attributable to HIV.
“Moreover, in all world regions, the contribution of HIV to cervical cancer falls disproportionately on younger women,†WHO said.
The Global strategy towards eliminating cervical cancer as a public health problem, adopted by the World Health Assembly in 2020, recommends a comprehensive approach to cervical cancer prevention and control.
The strategy, among others, proposes a vision of a world where cervical cancer is eliminated as a public health problem.
It proposes that 90-70-90 targets must be met by 2030 for countries to be on the path towards cervical cancer elimination.
That is; 90 percent of girls are fully vaccinated with the HPV vaccine by 15 years of age, 70 percent of women are screened with a high-performance test by 35 years of age and again by 45 years of age and 90 percent of women identified with the cervical disease receive treatment (90 percent of women with precancer treated, and 90 percent of women with invasive cancer managed).
Summary
- WHO country representative, Dr Richard Banda, said the annual report gives an overview of the WHO Lesotho country office’s undertakings and achievements in the context of an extraordinary health emergency.
- It further stated that women living with HIV were six times more likely to develop cervical cancer compared to women without HIV, and an estimated five percent of all cervical cancer cases were attributable to HIV.
- The Global strategy towards eliminating cervical cancer as a public health problem, adopted by the World Health Assembly in 2020, recommends a comprehensive approach to cervical cancer prevention and control.

Your Trusted Source for News and Insights in Lesotho!
At Newsday Media, we are passionate about delivering accurate, timely, and engaging news and multimedia content to our diverse audience. Founded with the vision of revolutionizing the media landscape in Lesotho, we have grown into a leading hybrid media company that blends traditional journalism with innovative digital platforms.